3 Reasons to Try Walk and Talk Therapy
Walk and Talk Therapy is just that—walking while talking with a trained therapist. It’s exercise but not cardio. Collaborative and professional. Walk and Talk is a useful modality for many people. Anyone suffering from anxiety, depression, coping with grief or loss, or feeling stagnant in life may find it beneficial.
I just hung up the phone with a colleague who wanted to pick my brain about providing Walk and Talk Therapy. Our call got me thinking about all the incredible benefits of this, seemingly to some, out-of-the box therapy, and why more people should consider trying it.
Walk and Talk Therapy is just that—walking while talking with a trained therapist. It’s exercise but not cardio. Collaborative and professional. Walk and Talk is a useful type of treatment for many people. Anyone suffering from anxiety or depression, coping with grief or loss, or those feeling stagnant in life may find it beneficial. This article talks about the benefits for new moms and also talks more about what Walk and Talk is, and what it isn’t (How walk and Talk Will Change Your Life, Mama).
Here are three MORE reasons to consider Walk and Talk Therapy:
Walk and Talk Therapy allows you to take small steps towards your goals. It’s a great metaphor. With each step, you’re moving forward in life, leaving your problems behind figuratively and literally. You’re no longer thinking about starting therapy, you’re engaging in it actively. You’re no longer thinking about exercise, you’re moving. Small steps change lives.
- You’ll feel Better—Both therapy and exercise are linked to improved mood and a decrease in symptoms of depression and anxiety. Physical exercise releases endorphins, which naturally spark positive feelings that help to reduce levels of depression and anxiety and prevent depressive symptoms. Being in nature is not only restorative but can improve your positive outlook on life and your ability to cope and recover from stress and illness. Walk and Talk Therapy leaves many people with improved self-esteem and sleep, and a greater overall sense of well-being.
- Hello multi-tasking! Life is busy, and carving out time for exercise, fresh air and your mental health can be daunting. Combining movement and therapy in nature is a convenient way to make progress in multiple areas of life that need tending. We've all heard sitting referred to as the new smoking. It’s not enough to just think about our need for more exercise, we need tools and plans that allow us to implement exercise in ways that don’t add greater stress to our lives.
If you’ve been thinking about starting or resuming counseling, could Walk and Talk would be a good fit for you? What do you think? Please chime in below in the comments section!
If you’d like to learn more about Walk and Talk therapy and live in San Diego, schedule your free 30 minute in-person consultation to find out if I might be the right fit for you!
3 Differences Between Postpartum Depression and The Baby Blues
People often confuse the Baby Blues and Postpartum Depression. Some like to say that all moms have a bit of postpartum. Have you heard that? When I hear that I presume they're not sure what the difference is between the Baby Blues, which are normal mood fluctuations after having a baby, and something more serious like Postpartum Depression or Postpartum Anxiety.
People often confuse the Baby Blues and Postpartum Depression. Some like to say that all moms have a bit of "postpartum". Have you heard that? When I hear that I presume they're not sure what the difference is between the Baby Blues, which are normal mood fluctuations after having a baby, and something more serious like Postpartum Depression or Postpartum Anxiety (and then there's the very important fact that "postpartum" is actually a period of time, not a condition).
For the purpose of this post, I want to clarify that PPD and PPA are NOT the only mental health concerns during pregnancy or postpartum. They fall under the umbrella of Perinatal Mood and Anxiety Disorders (PMAD), but I wouldn't have caught your attention with that title now, right?
Are there visual cues to detecting Postpartum Depression?
It's not only regular folks who are confused about the differences, but some medical professionals are also a bit unclear. I've heard that some some professionals specializing in women's health don't formally screen for perinatal mood or anxiety disorders because they feel they can tell whether a mom is struggling with PPD just by looking at her. Is it possible, you wonder?
Here's a quick quiz: below are two images of postpartum women. Which woman has the Baby Blues? Which has Postpartum Depression? If you're struggling with Postpartum Depression right now, or have in the past you know better than to fall for this one: you don't have to be sad and teary to be diagnosed with a PMAD. In fact, many women make an enormous effort to look put together. If this sounds like you, you're definitely not alone.
Image A
image b
The Face of the Baby Blues
The massive hormonal shift immediately after birthing a baby will more likely have you looking like the image on the left, "Image A" than the one on the right, "Image B". A shocker for many despite the fact that the Baby Blues affects up to 80% of mothers and as I said earlier, are due to a normal fluctuation of hormones.
Danielle Haines, on the left (Image A), is a doula and midwife in-training. She posted this raw image of herself on Facebook a few months ago. It was taken days after giving birth to her son, and she shared it in an effort to shed light on what the adjustment to early motherhood really looks like. Sadly, there's still stigma attached to this normal postpartum experience. Women are unfortunately hesitant to share that motherhood isn't all ice cream and roses.
The Face of Postpartum Depression
The image on the right, of course, is Hayden Panettiere. She looks like so many new moms--walking on the beach, seemingly happy with her baby and fiancé. No visual cues that she is suffering. This is also how many women who are suffering survive, by projecting a put-together image of themselves, avoiding the shame and stigma that still persists. Meanwhile they're falling apart on the inside. Alone. Because they "look fine" no one pays attention. They slip through the cracks. Up to 20% of women experience a Perinatal Mood or Anxiety Disorder.
When this photograph of Panettiere was captured her baby was three months old. She sought treatment for postpartum depression seven months(!) after that image was publicized. Fortunately, times are changing and celebrities like Hayden Panettiere are more open about their real-life experiences adjusting to early motherhood. Thankfully there is a growing effort to destigmatize PMADs, and to motivate others to get the help they need.
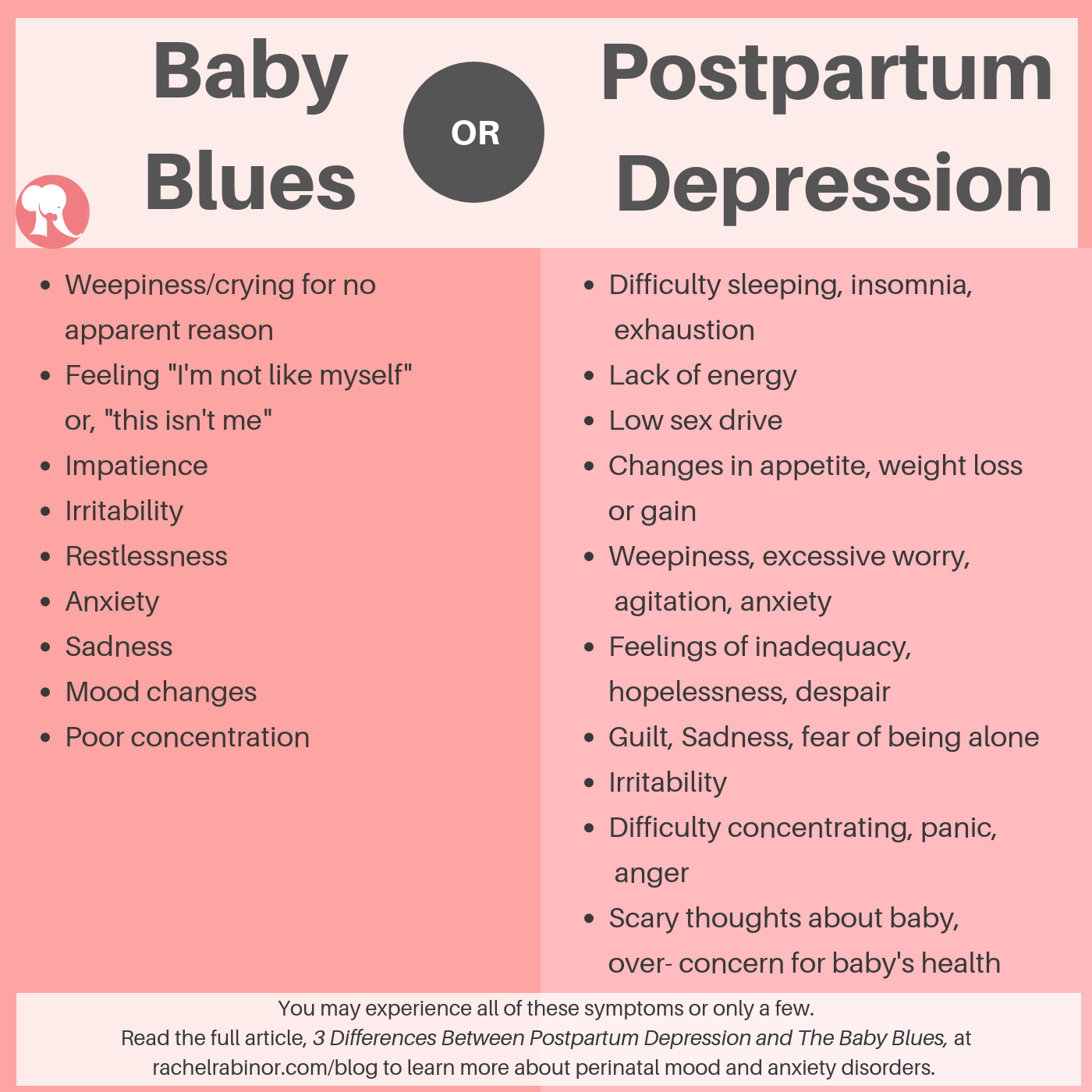
Symptoms of Postpartum Depression vs the Baby Blues
So if we (doctors included) can't tell by looking, how can we know if what we're feeling is part of the normal adjustment to early motherhood or something more serious? Below is a cheat sheet describing the different symptoms one may experience with either the Baby Blues or Postpartum Depression. You may notice some similarities. Keep reading below to better understand the differences.
It's not necessarily what you are feeling. It's how often you feel it, how long you have been feeling this way, and how much it impedes your functioning.
1-Duration
How long have you been feeling this way? The baby blues typically resolves within 2-3 weeks after giving birth, whereas Postpartum Depression symptoms continue for longer, and may present several weeks or months after having a new baby (*or bringing one home-- PPD impacts adoptive parents as well as fathers/non birthing parents).
2- Intensity
How much are these feelings interfering with your life? If you're not sure how to evaluate intensity, answer these questions:
Do I find it hard to care for my own basic needs or those of my baby or other children? Is my eating or sleeping affected by these feelings?
Are these feelings interfering with other important relationships? With my partner? Other family members? Friends? Work?
3-Frequency
How often are you feeling this way? Once a week? Once a day? Nonstop? There's a difference.
It's important to recognize that some of the most common symptoms of postpartum depression-- rage and anxiety for example-- look nothing like the stereotypical image of a saddened, depressed woman who can't get out of bed. Symptoms of the Baby Blues respond extremely well to rest and other forms of self-care. Here's an article that outlines 6 Ways to Improve your Postpartum Self-Care.
Getting help for Postpartum Depression
If you've been struggling with distressing thoughts and feelings for longer than two weeks, I recommend that you reach out to your doctor or a psychotherapist who specializes in perinatal mood and anxiety disorders.
And if it's less than two weeks but you just "know" something's not right, pay attention to that inner voice. Trust that you know yourself best and reach out for help. It really doesn't matter what we call it; you and your baby both deserve the care and attention you need to thrive. It's also important to reiterate that Postpartum Depression as referred to in this article, falls under the umbrella of perinatal mood and anxiety disorders, PMADs, which encompass other illnesses such as postpartum obsessive compulsive disorder, postpartum anxiety, postpartum post-traumatic stress disorder and postpartum psychosis.
If you or someone you know is struggling with a Perinatal Mood or Anxiety Disorder, please reach out for support. PMADs are very treatable. In my private practice in San Diego, California where I specialize in Maternal Mental Health, I offer a free 30 minute in-person consultation to find out if I'm the right therapist for you. Postpartum Support International (PSI) is a national organization that maintains a warmline and a list of trained providers specializing in Maternal Mental Health. If you’re in San Diego, CA, The Postpartum Health Alliance is our local chapter of PSI and a wonderful resource.
You Think Someone You Love Has PPD? Why YOU Need to Speak Up!
If you don’t speak up, the person you love might not get the help they need! Many women suffer in silence. Too many. More than 20 percent of moms are diagnosed with PPD; however, a recent study by BabyCenter shows that 40 percent do not seek medical help they need due to feelings of embarrassment, guilt and the expectation that they can get over it without professional help. There are many risks to mom and baby if postpartum depression or anxiety goes untreated, including:
Last week I got together with a new friend, Shelly, for a walk. When she learned more about the work I do with new and expecting mothers, the worry poured out of her. Shelly’s sister-in-law (SIL) had a baby 8 months ago, and she’s concerned about her. She's tired, irritable, incredibly anxious and doubting herself all the time (Yes, these are also symptoms of PPD--scroll to the bottom of this page for other symptoms you may not know about). Specializing in Maternal Mental Health, it’s par for the course to hear about sisters, friends, daughters and co-workers who are struggling with Postpartum Depression.
One in seven women deal with Perinatal Mood and Anxiety Disorders (PMADs), so really, it’s no surprise to hear about it so often. The thing that routinely does surprise me, however, is the hesitation many people share about approaching those they love with their concerns. This was Shelly to a T. She felt close to her SIL, but was apprehensive about recommending that she seek out some support.
Hesitant to offer support?
The more we talked the more I understood what was getting in Shelly’s way of reaching out. Shelly's the mom of a toddler and seems to have it together-- or together enough. She has a stable partner, family close by, a new business she’s passionate about; she’s confident and happy in her life. Her SIL, on the other hand, lives far from family and is further isolated by her husband’s current deployment with the Navy. She has a history of depression and other risk factors associated with PMADs.
By the end of our walk, I had a pretty clear grasp on Shelly’s hesitation to reach out to her SIL. She didn’t want her to feel judged, or less-than, by addressing concerns about her ability to cope with the adjustment to motherhood: A transition that has come fairly easily for Shelly. Shelly was also concerned about providing the right kind of support. With a history of depression, it was routine for family to jump in to “help” her SIL, and make everyday tasks easier. Her depression would subside for a bit and then the pattern would repeat. While a supportive family can be ideal in helping someone through their recovery, professional treatment may still be needed to address issues that may be contributing to the depression on a deeper level. Shelly wanted to help but she wasn’t sure how to do so effectively.
Why it’s important for YOU to speak up
If you don’t speak up, the person you love might not get the help they need! Many women suffer in silence. Too many. More than 20 percent of moms are diagnosed with PPD. However, a recent study by BabyCenter shows that 40 percent don't seek the medical help they need due to feelings of embarrassment, guilt and the expectation that they can get over it without professional help. There are many risks to mom and baby if postpartum depression or anxiety goes untreated.
RISKS OF NOT GETTING HELP WITH PPD
Risks to mom
- Lower quality of life
- Decreased ability to function at home or at work
- Risk of recurrent depression
- Suicide
Risks to baby
- Insecure attachment to mother
- Interference in cognitive development
Family stress and discord
Decreased care or neglect of other children
Loss of job/income
Also quite common is that women don’t even realize that what they’re experiencing isn’t normal! Just today I saw a third-time mom who started to recognize in my office that she had probably struggled with postpartum depression with her first two children without knowing. Sounds unbelievable but it’s true. The messages that women hear about motherhood reinforce that it’s natural, easy. That yes, you may be tired, but that’s normal. There’s a lot of grey area and it’s not always crystal clear whether what you’re experiencing is a normal adjustment to motherhood or something more serious. So if you notice something doesn’t seem right in someone you care about—Say something!
What to say to someone with Postpartum Depression
Shelly is a great example of someone who really wants to support someone they love, can identify their struggle, and for various reasons isn’t sure how to help. The reality is, it may not be the easiest conversation to have. But I find that women who are struggling are usually relieved to learn that there’s help available and that they don’t need to suffer in silence. Here’s a few suggestions of how to start the conversation:
1. Be direct
It’s important to be empathic, but it’s most important to be direct. Let her know that you’re worried about her; she doesn’t seem like herself. Let her know it’s normal, lots of women (1 in 7!) deal with PPD. It’s not uncommon for many women to go undiagnosed. Don’t let her slip through the cracks!
2. Be genuine
Speak from your heart. Let your love and care shine through. If she’s struggling to care for herself or her baby, this is serious. Remember, she’s not choosing to be neglectful, she’s struggling. You know she wants the best for her baby, for her family. Help her get the professional support she needs.
3. Be available
Make time for her. Once you connect her with people and resources she needs to improve her mental well-being, she will still need lots of support from people in her life who love her. She is vulnerable. Bring her food, go for a walk, watch her baby so she can take a shower. Keep her company.
If you or someone you know is struggling with a Perinatal Mood or Anxiety Disorder, please reach out for support. PMADs are very treatable. Postpartum Support International (PSI) is a national organization that maintains a warmline and also list of trained providers specializing in Maternal Mental Health. If you’re in San Diego, CA, The Postpartum Health Alliance is our local chapter of PSI and a wonderful resource.
How Walk + Talk Therapy Will Change Your Life, Mama
I know what it’s like to have a new baby around the house. The dirty dishes piled high, the never ending laundry, did you eat today? Just forget about exercise, you don’t even have time for a shower, right? You’re wondering if and when life will ever resemble those incredible Instagram photos you posted from your babymoon.
I know what it’s like to have a new baby around the house. The dirty dishes piled high, the never-ending laundry, did you eat today? Just forget about exercise, you don’t even have time for a shower, right? You’re wondering if and when life will ever resemble those incredible Instagram photos you posted from your babymoon.
This is a typical scenario for a family going through the transition to parenthood, yes? Of course there are precious moments, but it’s intense. That first year of life is nothing short of a hurricane sweeping through your world. When you factor in the inevitable additional emotional stress parenthood brings, life is more challenging. You may know you want professional help in the form of counseling, but you just can’t figure out how to fit it all in.
ENTER WALK AND TALK THERAPY
A recent conversation with a friend reminded me that although I offer Walk and Talk Therapy sessions in my San Diego-based private practice, where I specialize in maternal mental health, many people are unaware of it’s existence.
In my work as a licensed psychotherapist, over the past 15 years I’ve found that Walk and Talk Therapy is helpful for clients who are going through life transitions, have anxiety, are experiencing some kind of loss or grief among other challenges. Mothers of young children in particular, seem to really gravitate towards this modality; it’s so easy to bring your baby and stroller and go. Walk and Talk Therapy combines traditional talk therapy with physical exercise. Want to know more?
So here's the skinny on what Walk + Talk is and what it isn't
Walk and Talk Therapy is:
- a great option If you don't enjoy all the eye contact inherent in traditional office-based psychotherapy sessions.
- helpful if you're suffering from phobias, excessive anxiety, or are newly postpartum and not sure how to fit exercise of any kind back in your life.
- an opportunity to breathe fresh air and connect with nature (and another adult who happens to be trained to support your mental health)
Walk and talk is not:
- a cardio workout.
- strenuous.
- the same thing as chatting with a friend while walking.
Sounds pretty good so far, yes? Walking side by side with a trained psychotherapist feels collaborative and encourages conversations. Clients often feel more at ease sharing personal information in this informal, outdoor environment than traditional office-based therapy. Some clients also find it less intimidating to talk to a therapist when you’re both doing something else. And be assured, your confidentiality will be maintained, just as if you were in an office.
Here’s how Walk + Talk therapy will change your life, mama
1. You will feel better
Participating in regular Walk and Talk Therapy sessions with a trained therapist has been shown to reduce anxiety and tension, improve mood and increase energy. Physical exercise releases endorphins (feel-good hormones), which naturally trigger positive feelings helping to reduce levels of depression and anxiety, and can actually help prevent depressive symptoms. Many people report improved self-esteem and feelings of well-being, improved sleep (clearly that research wasn’t conducted on parents of young children), and an enhanced mind-body connection
2. You get to move your meat (aka exercise) AND take care of your mental health
It’s hard to fit in exercise as a new mom, or even an experienced one. Sure you could get a fancy jogging stroller but just the logistics of it all seem overwhelming. So here’s an opportunity to start small while also improving your mental health. Although Walk and Talk Therapy isn’t a workout, it is exercise and it can help you start to carve out time for what’s important.
3. You don’t need childcare
Enough said.
4. You will feel better
I already said this one but it’s worth repeating. As a new mother, it’s not uncommon to put everyone else first. After all, you have a new being that’s relying on you. But like they say on an airplane- you need to put your own oxygen mask on first before helping others. Self-care is important. If you don’t take care of you, not only will you suffer, but those you love will too.
If you’re struggling with your adjustment to motherhood, please reach out for support. Contact your doctor, Postpartum Support International, or a mental health professional. If you have more questions about Walk + Talk Therapy, or think it may be a good fit for you, check out these Frequently Asked Questions. And if you're in San Diego, give me a call!
How to Find a Therapist in San Diego
In San Diego, we’re lucky to have so many mental health practitioners. If only everyone in all corners of the globe were as fortunate as we are; choice is certainly a luxury. But having so many choices can also make it a challenge to find a counselor when you need one most. Typically you find yourself searching for a therapist when things aren't going so well, when you really need that extra bit of support. And with so many possibilities, you’re probably wondering— how do I choose!? Where do I start?
In San Diego, we’re lucky to have so many mental health practitioners. If only everyone in all corners of the globe were as fortunate as we are; choice is certainly a luxury. But having so many choices can also make it a challenge to find a counselor when you need one most. Typically you find yourself searching for a therapist when things aren't going so well, when you really need that extra bit of support. And with so many possibilities, you’re probably wondering— how do I choose!? Where do I start?
Below are a few recommendations for finding a counselor that’s right for you. There are many many qualified and capable therapists here in San Diego, the task is to find someone for YOU. The good news is that with so many options there’s bound to be someone who you can connect with and confide in. It will take some work on your end, but it will be well worth it!
Let's start with the logistics of finding a counselor in San Diego:
- Define your needs. Think about what you need from a therapist. Concretely– someone close to home, work, evening hours, morning hours, takes insurance, doesn't; has experience working with postpartum issues, infertility, anxiety, depression, parenting concerns…
- Look to your friends. When I need an ENT, a dentist, a car mechanic, I ask my friends for suggestions. Likewise, when I'm searching for a therapist for myself I also see if one of my besties has someone to recommend. But sometimes you're dealing with an issue that your friends haven't dealt with, or you're just not comfortable asking around. In that case, move on to my next suggestion.
- Head to the internet. Psychology Today is probably the most popular website with nationwide provider listings along with a smattering of everything for your psychological mind. Mental health providers post their info and you, the consumer can peruse at your leisure. There are a variety of filters you can activate to find someone who fits your search criteria. For example, if finding someone who’s close to your home is important, you can plug in your zip code and narrow down your choices instantly. You can also filter by gender, specialty, language... You get the idea. Another good place to search for a therapist is through specific associations that support the issue you’re struggling with. So if you want someone who’s experienced with infertility, for example, you will probably stumble across Resolve, which is the National Infertility Association. So even a national organization can point you to a local therapist through their provider listings.
- More internet research. So once you have some names, regardless of whether it came from a friend, Psychology Today, or Resolve, now's the time to learn more and review their website. You can read the “About” and Specialty pages, and look over the FAQs to get a feel for the counselor and see if he or she might be a good fit for you.
- Making Contact. Once you have 3 or 4 therapists that you’d like to get to know more, start making calls and sending emails. Many therapists in San Diego offer a free 15 – 20 minute phone consultation. It’s a great opportunity to ask questions and get a sense of whether this person may be able to help you before scheduling that first appointment.
- Meeting your therapist. You might want to schedule a couple of in-person appointments before deciding on a therapist. This is a great opportunity to ask more questions. Remember, you are interviewing this person to see if you want to hire them. Yes, you are hiring your therapist to help you through a difficult time, explore a specific issue, help manage challenging behaviors, etc. Pay attention to how patient they are with the process and your questions. How do you know you'll be able to work with someone? That is such a personal and individual thing– and a lot of it depends on knowing yourself and trusting your gut.
It is widely believed that the therapeutic relationship between you and your therapist is the most important factor in successfully resolving your presenting issue. The therapeutic relationship is the collaborative relationship between client and therapist, entirely focused on the client, to gain understanding of and effectively change the client in a way that supports their overall well-being.
The ability of the therapist to facilitate a strong working therapeutic relationship is everything. Theoretical orientation may be of interest to you, but as far as resolving the issue that brought you to therapy, it’s the counselor's innate abilities that matter most.
Below are some things to consider during your initial phone consultation and throughout the initial sessions of therapy to determine if someone might be a good therapist for you:
- Do you feel the therapist is genuinely engaged with you, focused on your well-being and motivated to help guide you? Does he or she remember to follow up or discuss topics further that you feel require more attention?
- Are you comfortable with the therapist? Are you able to share personal information and express yourself emotionally? Do you feel the conversation is insightful? Do you feel you can trust the therapist? Can you comfortably express your concerns and doubts with the counselor or is there some fear of judgment?
- Do you find the therapist comforting, empathic, and compassionate? Is he or she responsive to your emotional and verbal expressions? Are they cold when working with you?
These are just a few important aspects within the therapeutic process to pay attention to when trying to find a new therapist in San Diego. Hopefully you're feeling ready now to begin your search.
If you’re wondering if I'm a good match for you, call me for a free 20 minute phone consultation.